A $200B Opportunity for Policymakers and Entrepreneurs
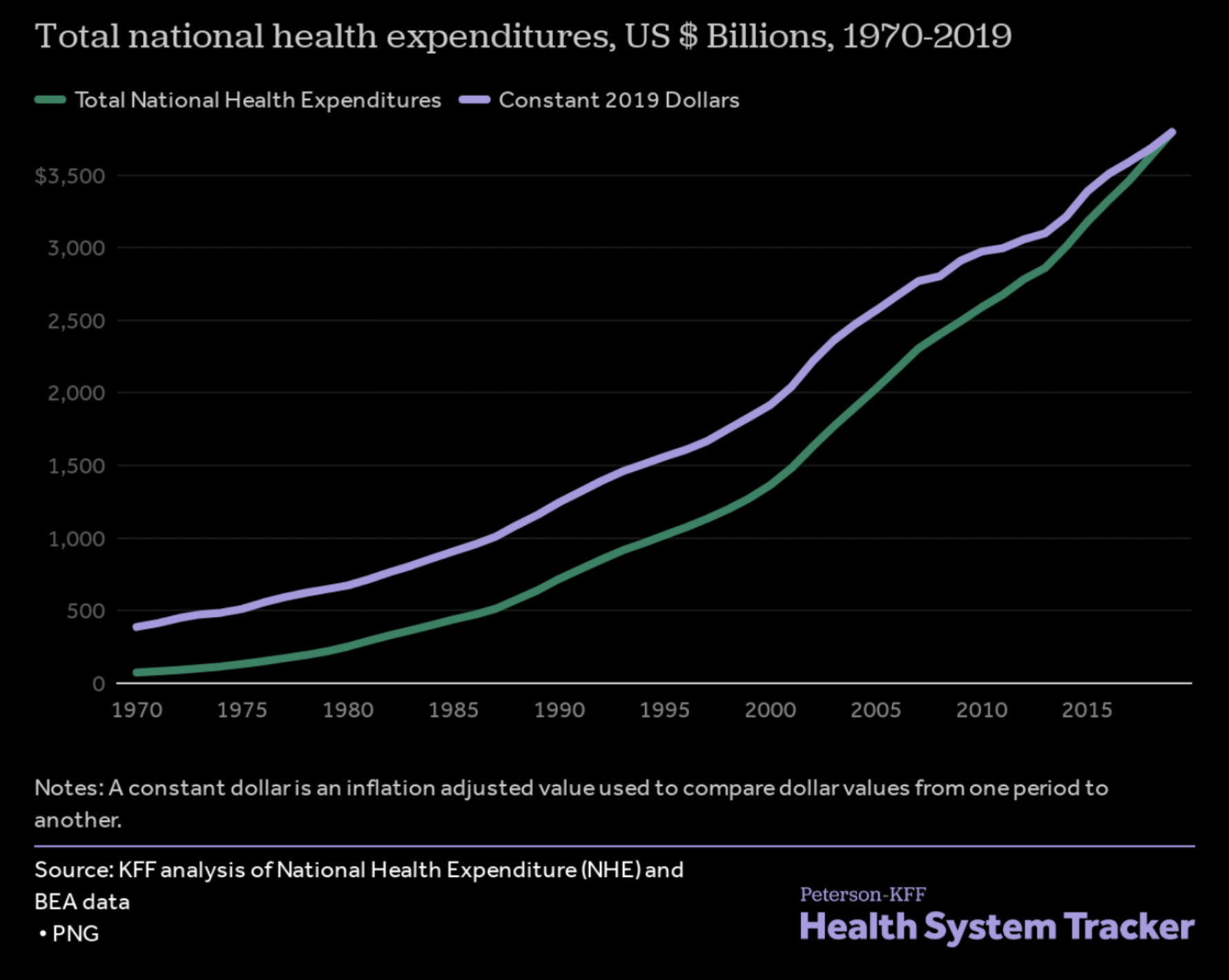
Since we published our proposal on “How to Save $900B Annually in American Healthcare” three years ago, the crisis facing the US healthcare system has deepened. Spending continues to grow at twice the rate of GDP, reaching $3.8 trillion in 2019 even as health outcomes stagnate.[1] This steady rise in expenditures is an underappreciated danger to our country’s socioeconomic well-being. Spiraling healthcare spending is steadily driving up the cost of living for working class Americans and, left unchecked, will create a fiscal emergency for state and federal governments.
Peterson-KFF
Fortunately, reeling in spending and improving health outcomes doesn’t need to be a zero-sum trade-off. We have the tools to fix our broken healthcare system. Emerging technologies offer the chance to deliver better care at dramatically lower price points. Policy reforms can reduce the staggering ~$935 billion in annual waste that plagues the healthcare system.[2] Political and business leaders have the responsibility to pursue both of these avenues to give Americans the care they deserve without sacrificing our nation’s future.
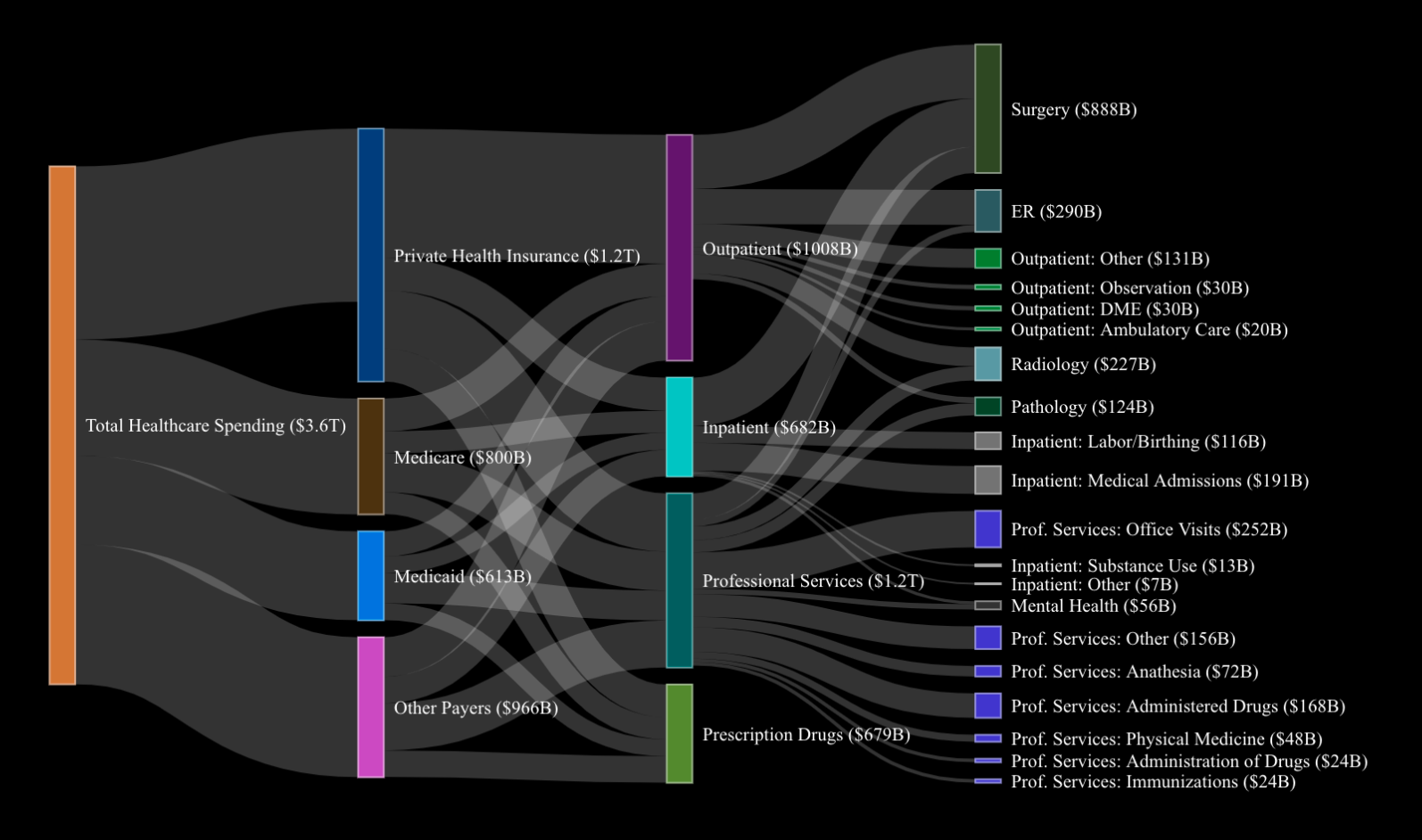
Flow of Spending in the American Healthcare System
In “How to Save $900B Annually in American Healthcare,” we outlined broad reforms that would bring down costs by aligning incentives across the healthcare system. This whitepaper hones in on specific areas where exciting new technologies combined with better steerage by private and public payers can deliver meaningful savings if entrepreneurs and policymakers are willing to take up the challenge. At 8VC, we are thrilled to partner with founders building ambitious companies in these spaces. At the Cicero Institute, we have made healthcare a priority, supporting reforms such as reference pricing for state employee health plans and creating a pathway for foreign-trained physicians to practice in the US.
Here are some concrete actions that can save US healthcare $200 billion annually:
1. Radiology ($17-24 billion in annual savings)
Annual Spend:
$227 billion
What To Do About It:
20-50% of radiological images fail to provide any incremental value for patients, either due to image duplication or human error.[3] Radiology’s highly manual workflows present a massive opportunity for healthcare entrepreneurs. Physicians cannot and should not be fully replaced by technology. However, an “iron man suit” that gives physicians superpowers in data sharing, image analysis, and task management could create $7-14 billion in savings by mitigating image overutilization, increasing productivity, and lowering labor costs.
Thanks to recent advances in artificial intelligence (AI), this vision isn’t a matter of speculation: start-ups like Nines and Sirona are developing products today that arm physicians to analyze images faster and better while minimizing burnout and waste. With the help of AI tools, radiologists can reliably identify the key features of a chest x-ray in 10 seconds.[4] On their own, humans might require 15 to 20 minutes for the same task. Likewise, the workstations that enable rapid image analysis can double as health information exchange systems that slash the chance of image duplication by 50%.[5]
An additional channel for savings would be to shift where patients receive radiological care. 60% of imaging takes place in hospital settings even though equivalent radiological imaging in outpatient clinics can be performed at less than half the cost.[6] Medicare could start reimbursing hospitals at the outpatient rate for radiology imaging procedures that can be reliably moved to clinics, reducing spending by at least $10 billion.
Promising Companies:
Nines AI, Sirona Medical, Aidoc, Zebra Medical Vision
2. Surgery ($40-60 billion in annual savings)
Annual Spend:
$888 billion
What To Do About It:
As with radiological imaging, hospital-affiliated facilities generally charge far more for services than unaffiliated outpatient facilities like clinics, independent physicians, and ambulatory surgery centers (ASCs). Price differentials are especially egregious for surgeries: private payers and Medicare often reimburse hospitals at twice the rate negotiated with ASCs located a short drive away. Yet, there is no difference in care quality between the two facility types. Not only are ASCs less prone to the monopolistic behavior of hospitals, but they have also been at the forefront of new reimbursement models (such as bundled payments) that motivate providers to take responsibility for a patient’s entire episode of care rather than simply billing them for discrete services (as occurs in fee-for-service payment models). In short, growing the number of surgeries performed at ASCs benefits patients and payers alike.
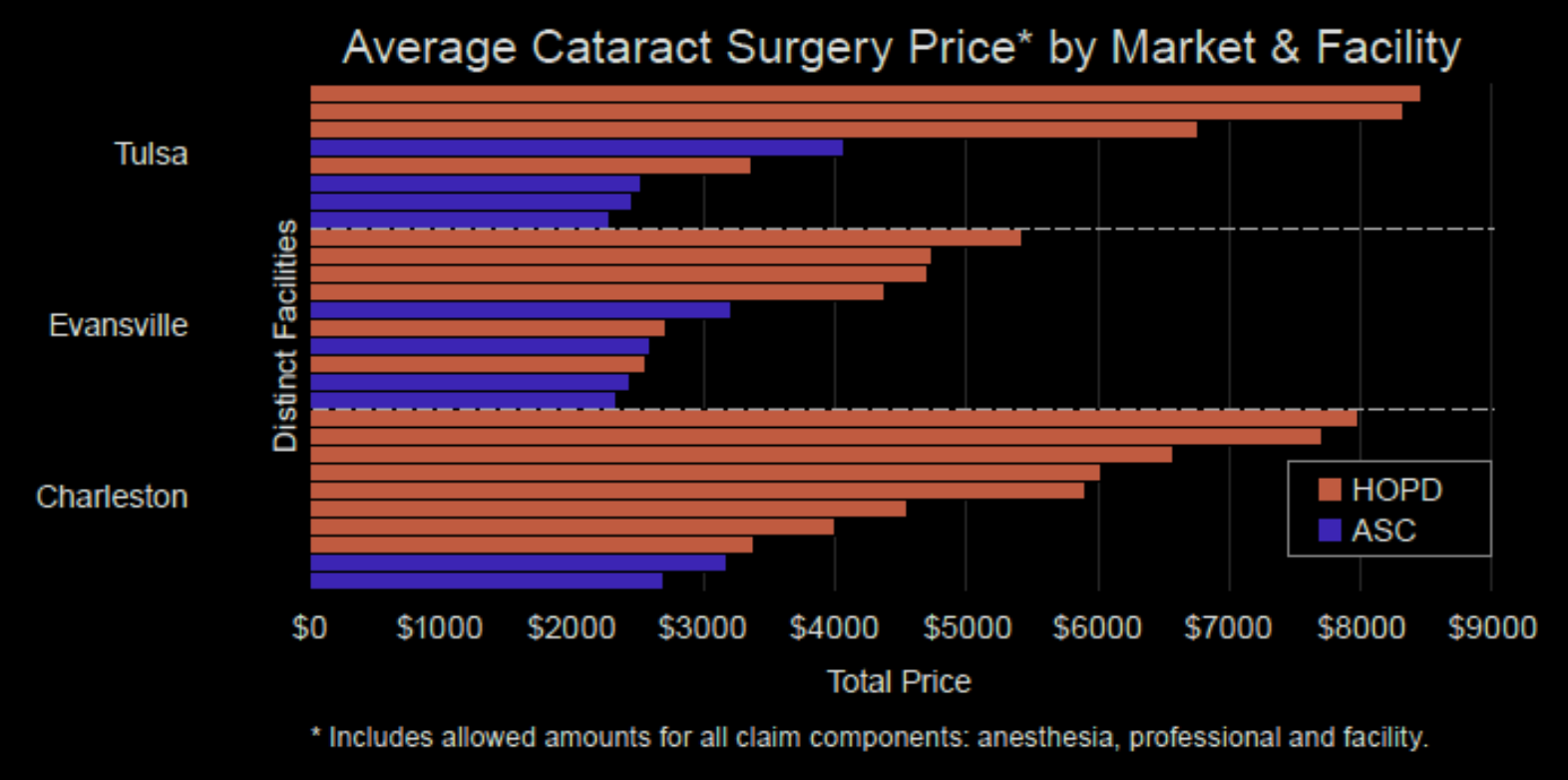
ASCs have steadily increased their market share over the last two decades and now perform more than half of all outpatient surgeries. This positive trend has already saved the healthcare system $40 billion a year.[7] Still, as of 2016, only 48% of surgeries that could be safely performed at ASCs took place in these facilities (with the rest occurring at hospital inpatient and outpatient departments).[8]
Migrating eligible surgeries to ASCs could realize meaningful savings. Further efforts by payers like UnitedHealthcare to purchase and expand ASCs is one promising path. Medicare could also begin to reimburse hospitals at the same rate as other outpatient facilities for surgeries that are commonly performed in ASCs. These changes would save the healthcare system $40-60 billion per year.
Promising Companies:
Healthcare Outcomes Performance Company, CORE Institute, Remedy, Surgery Center of Oklahoma, orthopedic ASCs
3. Birthing ($2 billion in annual savings)
Annual Spend:
$116 billion
What To Do About It:
America is the most expensive nation for mothers to give birth: the average cost to deliver a child is about $30,000.[9] For uncomplicated deliveries (60-90% of births), birthing centers offer a high quality alternative to hospitals at a far lower price point.[10] These facilities can save payers $1100 per birth by providing virtual prenatal care, supplementing OB-GYNs with midwives, avoiding unnecessary c-sections, administering cheaper drugs to expectant mothers, and relying on fewer expensive (and often unnecessary) post-birthing services.[11] Payers should encourage women with a low risk profile (1.5-2 million births each year) to plan to deliver at birthing centers for a more comfortable, personalized, and cost-effective experience. This shift could yield up to $2 billion per year in cost reductions.
Promising Companies:
Oula Health, Maven Care, Quilted Health
4. Pathology ($13-20 billion in annual savings)
Annual Spend:
$124 billion
What To Do About It:
Pathology departments are beset by long turnaround times, low digitization rates, and a lack of coordination across laboratories. Providers can streamline this waste by adopting technology workflows pioneered by companies such as PathAI and Prosica. PathAI is pairing physicians with AI tooling to enable less labor-intensive, more accurate diagnoses. AI-assisted image analysis can diagnose certain types of cancer with just a 1.2% error rate – far better than the average 3% error rate for humans.[12] Any healthcare payer should leap at the chance to send patients to labs that cut diagnosis misses in half while simultaneously reducing spend.
Cancer pathology is a space where digital solutions (such as those created by Prosica) are likely to have outsized impact: a study from the National Institute of Health found that shifting to digital systems saved $5,000 in pathology costs annually for each cancer patient.[13] With 1.8M new cancer cases diagnosed annually, such a figure implies possible savings of about $7.7 billion. Applied more generally, AI and workflow automation products could reduce pathology spending by $13-20 billion.
Promising Companies:
PathAI, Prosica, Paige
5. End-Stage Renal Disease ($30B in annual savings)
Annual Spend:
$50 billion
What To Do About It:
End-stage renal disease afflicts nearly 800,000 Americans. Medicare covers all Americans suffering from this affliction, a responsibility that amounts to over 7% ($50 billion) of program expenditures.[14] Most patients undergo dialysis, a draining and unpleasant treatment that involves recycling blood through a dialysis machine for several hours three times per week.
Preventive care could save tens of billions of dollars and change hundreds of thousands of lives for the better by managing renal disease in its earlier stages. Assigning early-stage renal disease patients to nephrologists, for example, can substantially lower the probability of disease progression.[15] Perversely, however, payers have little financial motivation to engage in the interventions that forestall disease progress since the government will eventually assume financial responsibility for patients.
As we have written in the past, Medicare must rework these incentives. One promising step in this direction is Medicare’s Diabetes Prevention Program (DPP), which rewards providers for specific interventions that help at-risk patients lose weight and change their diets. DPP programs save Medicare $2120 per patient annually by measurably reducing the chance that patients develop diabetes. If applied to the entire population of Medicare beneficiaries at risk for end-stage renal disease, these programs could drastically improve Americans’ physical and financial health.
For patients already suffering from end-stage renal disease, kidney transplants offer a less expensive alternative to dialysis that also increases the likelihood of patient survival.[16] Migrating eligible Medicare beneficiaries from dialysis to kidney transplants could generate savings on the order of $20 billion. However, in addition to poor provider steerage practices, transplants have been constrained by an undersupply of kidneys. This tragic fact is a reflection of incompetence as well as true scarcity. Organ procurement organizations, government monopoly contractors charged with handling organs from deceased donors, lose 28,000 organs each year.[17] Decertifying organ procurement organizations that fail to meet minimum performance standards and ramping up production of bioartificial kidneys are two ways to unlock kidney supply (though the latter remain several years from mass clinical use).[18]
A more near-term solution to save Medicare $10 billion would entail moving patients from hemodialysis to peritoneal dialysis, a notably cheaper and equally effective form of treatment.[19]
Promising Companies:
Strive Health, Somatus, Cricket Health
6. Dual-Eligible Care ($50 billion in annual savings)
Annual Spend:
$470B
What To Do About It:
Our country fails to provide high-quality, affordable healthcare to the elderly. Currently available care options restrict senior patients’ ability to live freely: hundreds of thousands are forced to live in nursing homes because they lack the means to reside safely in their own homes.
Programs of All-Inclusive Care for the Elderly (PACE) care offer a superior, low-cost model where low-income seniors can receive excellent care at technology-enabled medical and social centers without needing to abandon their homes. PACE enrollees experience 24% lower hospitalizations and 16% lower readmissions compared to other dual-eligible seniors. PACE centers can also achieve efficiencies that lower Medicaid expenditures for seniors by 13%.[20]
Several companies, such as InnovAge, operate PACE businesses, but the space is highly underpenetrated. Only about 60,000 patients of the 1.8M eligible population are enrolled in PACE. Moving eligible seniors to PACE would save Medicaid $50B annually. To accomplish this goal, political leaders will need to reduce the regulatory complexity involved in setting up PACE facilities and push back against special interests such as skilled nursing lobbies that oppose reform.
Promising Companies:
InnovAge, Trinity Health PACE
7. End-of-Life Care ($19 billion in annual savings)
Annual Spend:
$380 billion
What To Do About It:
End-of-life care in the US is cripplingly expensive and uncomfortable for those in their final months. Patients pass in and out of hospitals for procedures that are painful rather than curative. Consequently, acute care for the 5% of beneficiaries who pass away each year amounts to 30% of Medicare expenditures. This model of care is callous and places a massive financial burden on younger generations. Yet, histrionic language about “death panels” has largely paralyzed reform.
Rather than mandating how these patients are treated, our society must give them the freedom to choose how they wish to spend their final months. Best-of-breed managed health organizations like Aspire Health empower the terminally ill to make these decisions, ensuring that they receive top-quality palliative care while shrinking costs by as much as $19 billion. In these organizations, care managers work with patients to decide what kind of care they wish to obtain and then coordinate across providers to reduce unnecessary procedures. Patients in programs like Aspire are 67% more likely to enroll in hospice than those receiving traditional care.[21] The result is a more humane model for end-of-life care that realizes savings north of $5000 per beneficiary.[22]
Promising Companies:
Aspire Health, Uphold Health
8. Claims Processing and Adjudication ($28 billion in annual savings)
Annual Spend:
$800 billion
What To Do About It:
The US spends $800 billion on healthcare administration each year, a far greater share than other developed countries.[23] A major driver of this overhead is the industry’s byzantine claims processing system. Physicians and hospitals hire legions of administrators who toil away at manually coding claims forms that they submit to payers for reimbursement. Payers then collect claims forms, standardize them, and review them for fraud or inaccuracy. The process is about as archaic and slow as it sounds, costing the healthcare system $150 billion each year.[24]
Automated medical coding and standardized, real-time claims submission could shrink this number by at least $10 billion. Start-ups such as Candid Health and Nym Health are building AI-enabled solutions that could increase claims processing throughput by an order of magnitude. Likewise, companies that build software to ingest individual provider claims forms and map them to a standardized form for payers would move the needle substantially on real-time claims submission.
In a similar vein, doctors and nurses waste untold hours on administrative activities like inputting data into EHRs, ordering tests, filling out prescriptions, and completing paperwork.[25] Software companies that reduce such administrative burdens will turbocharge physician productivity. Voice-to-text transcription start-up Nuance is one example of the kind of game-changing solutions that can be built here.
Together, standardized, real-time claims submission and administrative workflow software could drive $28 billion in savings for the healthcare industry.
Promising Companies:
Candid Health, Nym Health, Fathom Health, Ooda Health, Nuance
Conclusion
Reforming American healthcare is a battle for our nation’s future. Policymakers and entrepreneurs must take action to control spiraling costs by adopting promising innovations, aligning incentives, and steering patients towards less expensive and higher quality programs. Otherwise, rising expenditures will curtail economic mobility and spark vicious, zero-sum conflict. The $200 billion in savings opportunities identified in this piece provide a roadmap for our leaders to set America on a more sustainable course.
Joe Lonsdale
General Partner, 8VC
Philip Clark
Chief of Staff to Joe Lonsdale, 8VC
[1] “Health System Tracker: How Has the Quality of the US Healthcare System Changed Over Time?.” Peterson-KFF. April 19, 2019. https://www.healthsystemtracker.org/chart-collection/how-has-the-quality-of-the-u-s-healthcare-system-changed-over-time/#item-start.
[2] William Shrank, Teresa Rogstad, Natasha Parekh. “Waste in the US Health Care System Estimated Costs and Potential for Savings.” JAMA. October 7, 2019. https://jamanetwork.com/journals/jama/article-abstract/2752664.
[3] William Hendee, et al. “Addressing Overutilization in Medical Imaging.” Radiology. October 1, 2010. https://pubs.rs
[4] Jessica Kent. “Artificial Intelligence System Analyzes Chest X-Rays in 10 Seconds.” Health IT Analytics. September 30, 2019. https://healthitanalytics.com/news/artificial-intelligence-system-analyzes-chest-x-rays-in-10-seconds
[5] Michael Bassett. “Study finds that HIE reduces duplicate imaging, provides cost savings.” Radiology Business. February 4, 2015. https://www.radiologybusiness.com/topics/economics/study-finds-hie-reduces-duplicate-imaging-provides-cost-savings.
[6] Jamie Cleverley. “Identifying the Gap Between Hospital and Free-Standing Prices.” Health Financial Management Association. https://www.hfma.org/topics/article/52656.html.
[7] Tim van Biesen and Todd Johnson. “Ambulatory Surgery Center Growth Accelerates: Is Medtech Ready?” Bain & Company. September 23, 2019. https://www.bain.com/insights/ambulatory-surgery-center-growth-accelerates-is-medtech-ready/
[8] “Study: Commercial Insurance Cost Savings in Ambulatory Surgery Centers.” Advancing Surgical Care. https://www.ascassociation.org/advancingsurgicalcare/reducinghealthcarecosts/costsavings/healthcarebluebookstudy.
[9] “Investing in Entrepreneurs that Improve Healthcare.” FCA Venture Partners. https://static1.squarespace.com/static/59244cb9db29d6a7b99e8006/t/5ddd89e6377ff72cee41b32b/1574799849113/FCA+Birth+Center+Report+-+vF.pdf.
[10] Roosa Tikkanen et al. Maternal Mortality and Maternity Care in the United States Compared to 10 Other Developed Countries.” The Commonwealth Fund. November 18, 2020. https://www.commonwealthfund.org/publications/issue-briefs/2020/nov/maternal-mortality-maternity-care-us-compared-10-countries.
[11] Embry Howell et al. “Potential Medicaid Cost Savings from Maternity Care Based at a Freestanding Birth Center.” Medicare Medicaid Res Rev. 2014. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4167228/.
[12] K.S. Wang et al. “Accurate diagnosis of colorectal cancer based on histopathology images using artificial intelligence.” BMC Medicine. March 23, 2021. https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-021-01942-5#Bib1.
[13] Jonhan Ho et al. “Can Digital Pathology Result In Cost Savings? A Financial Projection For Digital Pathology Implementation At A Large Integrated Health Care Organization.” NIH. August 28, 2014. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4168664/.
[14] “Healthcare Expenditures for Persons with ESRD>.” USRDS. https://usrds.org/media/1734/v2_c09_esrd_costs_18_usrds.pdf.
[15] Lee et al. “Effects of proactive population-based nephrologist oversight on progression of chronic kidney disease: a retrospective control analysis.” BMC Health Services Research. 2012. https://pubmed.ncbi.nlm.nih.gov/22894681/.
[16] Jeff Zaltzman- Pro. “This house resolves that kidney transplantation is better than dialysis.” St. Michael Hospital. https://www.stmichaelshospital.com/pdf/programs/renal-transplant/transplant-vs-dialysis.pdf.
[17] JoNel Aleccia. “How Lifesaving Organs For Transplant Go Missing In Transit.” KHN. February 10, 2020. https://khn.org/news/how-lifesaving-organs-for-transplant-go-missing-in-transit/.
[18] The new CMS rules to hold organ procurement organizations to account is a step in the right direction, but they will not take effect until 2022 and no organ procurement organization could lose its government contract until 2026.
[19] “Peritoneal Dialysis: What You Need to Know.” National Kidney Foundation. https://www.kidney.org/atoz/content/peritoneal.
[20] National Pace Association. https://www.npaonline.org.
[21] Peter Ubel. “Reducing End-Of-Life Costs. It’s Not A Futile Pursuit.” Forbes. Feb 28, 2020. https://www.forbes.com/sites/peterubel/2020/02/28/reducing-end-of-life-costs-its-not-a-futile-pursuit/?sh=22e45c493285.
[22] Brad Stuart, Elizabeth Mahler, and Praba Koomson. “A Large-Scale Advanced Illness Intervention Informs Medicare’s New Serious Illness Payment Model.” Health Affairs. June 2019. https://www.healthaffairs.org/doi/full/10.1377/hlthaff.2018.05517.[23] David Himmelstein, Terry Campbell, Steffie Woolhander. “Health Care Administrative Costs in the United States and Canada, 2017.” NIH. January 21, 2020. https://pubmed.ncbi.nlm.nih.gov/31905376/.
[24] Peter Orszag and Rahul Rekhi. “Real-Time Adjudication for Health Insurance Claims.” Lazard.
[25] Linda Carroll. “More than a third of U.S. healthcare costs go to bureaucracy.” Reuters. January 6, 2020. https://www.reuters.com/article/us-health-costs-administration/more-than-a-third-of-u-s-healthcare-costs-go-to-bureaucracy-idUSKBN1Z5261.

